Whether you have PCOS or not, if you have been trying to conceive for more than 12 months or you are over the age of 35 years then you should consider seeing your doctor for fertility investigations.
 The aim of fertility testing is to rule out any possible cause that could be reducing or stopping your chances of a pregnancy ( Also have a read of the fertility problems). Both you and your partner should be tested. It is no use just testing you and not him. It may seem a frightening time and many of my patients have voiced their concerns about the fear that “at the back of their mind, they may be the problem”, or are worried that their partner may react negatively.
The aim of fertility testing is to rule out any possible cause that could be reducing or stopping your chances of a pregnancy ( Also have a read of the fertility problems). Both you and your partner should be tested. It is no use just testing you and not him. It may seem a frightening time and many of my patients have voiced their concerns about the fear that “at the back of their mind, they may be the problem”, or are worried that their partner may react negatively.
Below are a series of fertility tests I recommend for my couples in my fertility clinic. Your family doctor can organise these for you.
Fertility Investigation: Blood Tests
Simple blood tests can be used to see where you stand right now in regards to hormone levels. They include:
- The pituitary hormones Follicle Stimulating Hormone (FSH) and Luteinising hormone (LH), and Prolactin (PRL) to determine if there are any hormonal issues affecting your fertility.
- The ovarian hormone level called ‘Progesterone‘ which will indicate if you are ovulating or not.
- Androgen Hormones are checked : Testosterone, DHEAS, and Free Androgen Index (FAI) to determine the possibility of Polycystic ovarian syndrome
- Thyroid hormones are checked as these are important for metabolic function.
- Ovarian Reserve testing using the hormone AMH:- Antimullerian hormone. This hormone can give an indication to the egg numbers a woman may have in her ovaries. It will be discussed further below
- Pre-pregnancy antenatal screening tests are also performed. These check for your immunity to chicken pox, German measles, hepatitis, as well as a Full blood count rule out anaemia
Once these basic blood tests are taken and the results reviewed, your fertility specialist will likely order a few more intensive tests on both partners to help determine why you may be having problems conceiving. Some of the most common procedures performed during fertility testing include:
The Pelvic Ultrasound
A pelvic ultrasound is the first step to checking a woman’s ovaries and uterus in her pelvis. It is a simple painless and non invasive test used to check for any abnormalities or obvious problems such as cysts on the ovaries, Polycystic ovaries or endometriosis, swollen fallopian tubes, benign lumps in the uterus called fibroids, or polyps within the uterus and more. All of which could affect a woman’s chances of conceiving. At the same time the radiographer can check a woman’s ovarian reserve by counting the antral follicles in her ovary.
Tests for Ovarian Reserve
A woman is born with a pool of approximately 1 million ovarian follicles, and during her years these follicles are continually lost through natural “timed cell death” called Apotptosis.
The number of remaining follicles in a woman’s ovary is called “The Ovarian Reserve”. There are 2 ways to look at your ovarian reserve, one is to perform a pelvic ultrasound and count the antral follicles in each ovary, and the other is a blood test that measures a hormone called Antimullerian Hormone …AMH for short. Both tests complement each other.
Ultrasound and Antral Follicle Count
As mentioned above this is a pelvis scan on your ovaries, where follicles show up as dark holes and can be counted in each ovary.
Antimullerian Hormone Levels AMH
AMH is a blood test. AMH is a hormone produced by the granulosa cells of the early antral follicles in the ovary and is called the ” Egg Timer Test”. As the number of eggs in the ovary declines with age, the blood AMH levels also fall.
A high level of AMH can indicate polycystic ovaries. A low level can give an indication of diminished ovarian reserve in women with declining fertility. AMH can be tested anytime in the menstrual cycle as the levels remain constant and do not fluctuate.
Fertility Investigation: Testing The Fallopian Tubes
1. Hysterosalpingogram (HSG) X-Ray
A hysterosalpingogram is an x-ray test performed as an outpatient in a radiology department, used to assess if there are any problems of the female anatomy including the cervix, uterus and fallopian tubes.
Special contrast dye is injected through the cervix into the uterus and fallopian tubes, the specialist can clearly see if there are any problems inside the uterus that could prevent an embryo from attaching/ implanting, and to check for blockages within the fallopian tubes, or other abnormalities that could be blocking conception. Pictures are taken using a steady beam of X-ray (fluoroscopy) as the dye passes through the uterus and fallopian tubes.
2. Hy-Co-Sy
A hycosy is another method for testing the openness of the fallopian tubes. It is performed using an ultrasound machine and placing a small amount of sterile water through the cervix into the uterus while scanning for the fluid to passs through the tubes. It does not take long, but the procedure may produce some cramping pain during and afterwards. I recommend to my patients to take 2 tablets of Nurofen or Naprogesic one hour prior to the procedure.
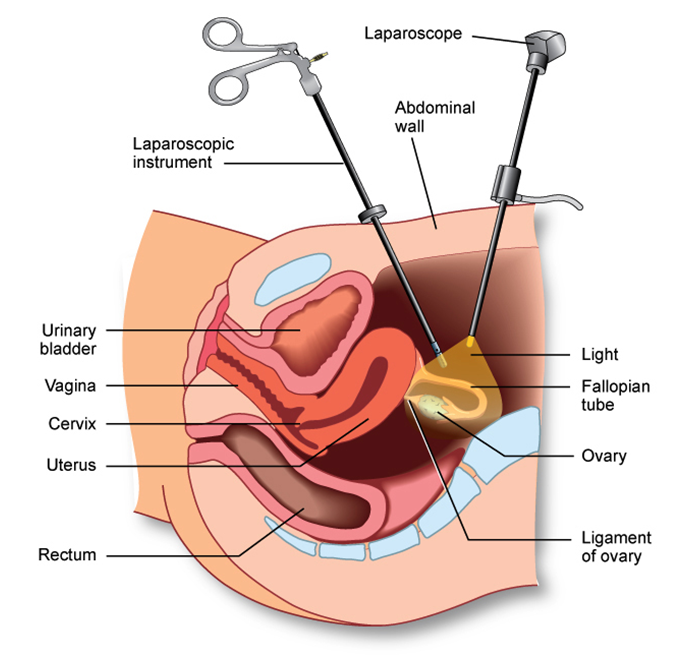
3. Laparoscopy and Dye
A laparoscopy is an operative procedure requiring a general anaesthetic and a short hospital admission. A thin telescope is inserted through the navel into the abdomen so the fertility specialist can visualise the pelvis including the uterus, ovaries and fallopian tubes. The Fallopian tubes can be tested by putting a blue dye through them to check if they are open and not blocked. At the same time problems such as endometriosis, pelvic adhesions and blocked swollen tubes and fibroids can be diagnosed and sometimes treated. (see fertility problems)
Figure: Laparoscopy
Testing the Uterus with a Hysteroscopy
This is a 20 minute day surgery procedure that requires you to be asleep. A thin telescopic camera is placed through the cervix into the cavity of the uterus to check for any problems such as polyps or fibroids or any changes in the lining of the uterus. It is often performed at the same time as a laparoscopy. A biopsy of the lining of your uterus is taken and sent off to pathology to rule out any infection or changes in the lining that could affect implantation of the embryo.
Fertility Investigations for Him
The Diagnostic semen analysis
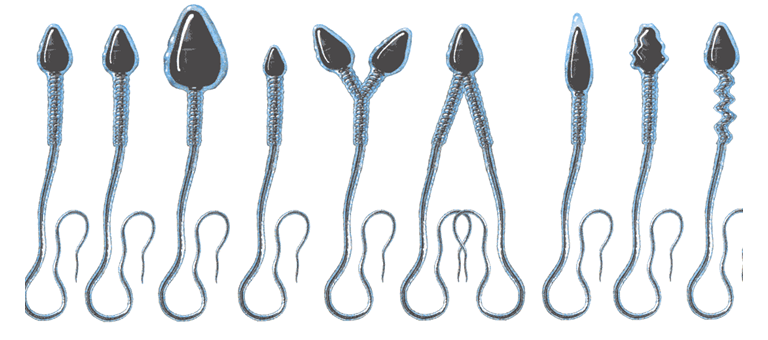
The main fertility test for men is the semen test. This is a simple test and involves the male partner giving a fresh sample of semen to an Andrology laboratory for testing. The results will help to understand whether factors affecting the sperm play a part in the reason why it may be taking longer to conceive. Under the microscope the lab assesses:
- To assess the Concentration of Sperm ……. that means how many sperm are present in the sample
- To assess the Motility of Sperm ………… that means to check if they are moving correctly and rapidly
- To assess the Morphology of the Sperm ………. which means look at the appearance of sperm and check and if there is a good percentage of them looking normal
- To check for the presence or absence of Antisperm Antibodies
- To check for any red blood cells or white cells that may indicate infection or other pathology
Sperm Culture
Sperm culture is the examination for microbes in the sperm. This involves the direct examination under a microscope of a sperm sample, followed by its culturing on a suitable medium for growing bacteria.
Semen DNA Fragmentation Studies
This is a complementary test to the semen analysis. The DNA fragmentation studies is a recently developed technique on semen that measures the damage of DNA in the head of the sperm, and gives a percentage value called DNA fragmentation Index or DFI for short.
The DNA is the sperm’s genetic material, and fragmentation signifies that some of the strands of DNA have been broken. If these breakages are not serious, then they can be repaired in the female egg/oocyte after fertilisation. However, above a certain level/percentage of breakages, this repair process is not possible at a sufficient level to allow the embryo to develop in a normal fashion.
A normal semen sample has less than 15% of the sperm with DNA damage. Men with poor fertility potential have greater than 30% of their sperm damaged. A DFI Between 16% and 29% is considered good to fair fertility potential but becomes poorer as it approaches 27%.
Standard DFI values:
- DFI <15% = good quality sperm DNA
- DFI =16 – 29 % = fair sperm DNA
- DFI > 30 % = very deteriorated sperm DNA
This deterioration of the sperm DNA is thought to be due to an excess of free radicals, and DFI increases with Male age, smoking, testes exposure to heat and toxins.